Navigating through menopause can often feel like maneuvering through a maze of physical and emotional challenges. One common obstacle that many women face is joint pain.
Aching joints can drastically reduce quality of life, making everyday activities a struggle. But rest assured, it’s not an insurmountable problem.
In this blog post, we will explore a variety of tips and techniques to help you relieve joint pain caused by menopause.
By understanding the causes and treatments, you can mitigate this discomfort and carry on with your life, unhindered by pain.
Menopause is a natural part of life, and it’s an opportunity for growth and empowerment. You are not alone on this journey, and with these valuable tips, you’ll be fully prepared to embrace the challenges ahead with confidence and grace.
How Does The Menopause Cause Painful Joints?
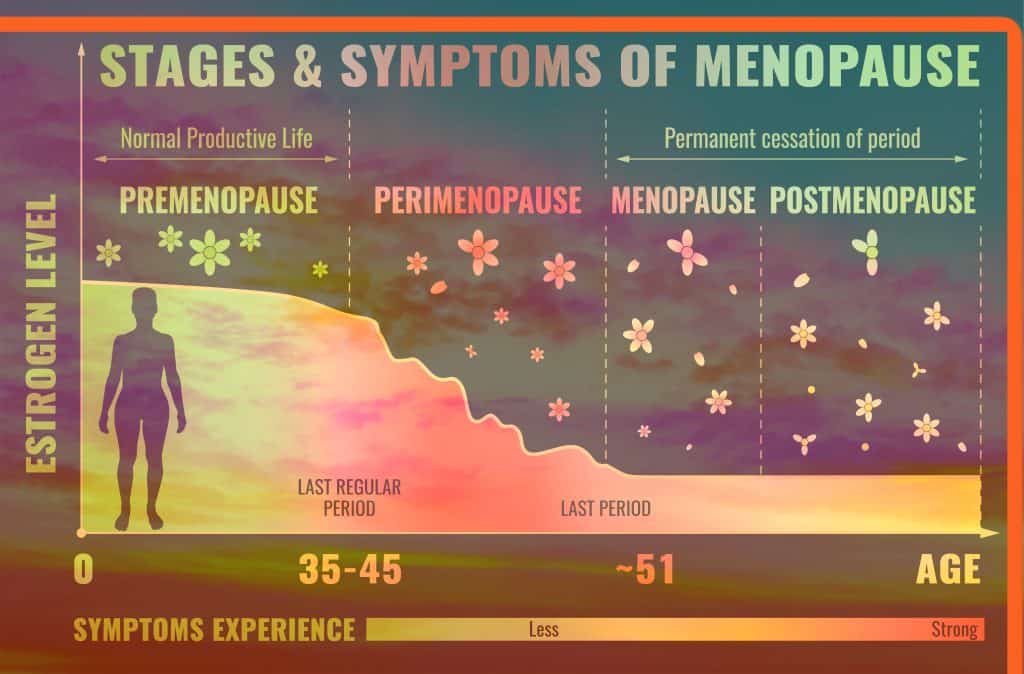
During menopause, the natural decline of oestrogen levels can have significant effects on your body, including causing joint pain.
Oestrogen plays a crucial role in maintaining healthy bones and joints, and a drop in this hormone can lead to an increase in inflammation, which in turn can cause joint discomfort and pain. However, there are ways to relieve joint pain during this phase.
Additionally, oestrogen helps regulate fluid levels, and when its levels decrease, it could result in joint stiffness and aching due to less lubrication.
Understanding these hormonal changes can provide a clearer picture of why joint pain can occur during menopause.
Lifestyle factors can also contribute to the onset of joint pain during menopause. As we age, changes in our daily routine, such as a decrease in physical activity and alterations in our diet, can exacerbate menopause-induced joint pain.
Incorporating anti-inflammatory foods into our diet and reducing the consumption of processed and fried foods can help alleviate joint inflammation and increase overall comfort.
Similarly, maintaining an active lifestyle can prevent stiffness and aching in joints. Regular physical activity helps keep joints flexible and strengthens the muscles that support them, thus relieving joint pain.
Relieve Joint Pain With Our Top 3 Tips!
Strength Training
Strength training is an effective strategy to relieve joint pain caused by menopause. This type of training involves working against resistance to build and strengthen muscles, which in turn offer enhanced support for the joints.
It’s essential to understand that strength training needs to be initiated gradually, especially if you’re a beginner.
Starting with light weights and slowly increasing intensity can help prevent potential injuries and ensure that you’re comfortably adjusting to the routine.
Incorporating strength training exercises into your regular routine can significantly relieve joint pain by providing your joints with stronger shock-absorbing muscles, reducing the stress on them.
Additionally, it can improve your overall body strength and flexibility, which further helps to relieve joint pain and enhances your general well-being.
Anti-Inflammatory Diet
Adopting a nutritious diet is an effective way to relieve joint pain associated with menopause. A balanced, wholesome diet not only helps maintain your overall health but can also significantly impact your joint health.
Including anti-inflammatory foods in your daily intake can work wonders in helping to relieve joint pain.
Foods rich in omega-3 fatty acids, such as salmon or flaxseeds, and antioxidant-rich fruits and vegetables, like berries and leafy greens, can reduce inflammation and thus help relieve joint pain.
Additionally, spices like turmeric and ginger possess potent anti-inflammatory properties that can help relieve joint pain.
Thus, eating a well-rounded diet, enriched with anti-inflammatory foods, is an excellent strategy to relieve joint pain caused by menopause.
Stretching
Incorporating a regular stretching routine is another effective method to alleviate joint pain during menopause. Stretching can help increase flexibility, reduce stiffness, and improve the range of motion in your joints.
For instance, gentle yoga poses such as the ‘Child’s Pose’ can stretch and relieve tension in the lower back, hips, thighs, and ankles.
Another beneficial stretch is the ‘Chest Stretch’, which can help combat the forward slump often associated with joint pain and improve posture by stretching the chest and shoulder muscles.
We recommend dedicating at least 20 minutes per day to stretching activities. Consistent practice can help increase joint mobility and decrease discomfort, aiding your journey through menopause with less pain.
Looking For Women’s Health Advice?
Here at Focus Osteopathy, we know it can be a little scary to take your health into your own hands, but that’s why we’re here!
We want to give people like you help with everything from aches and pains to their nutrition and healthy habits so that you can overcome whatever life throws at you and enjoy every single day feeling healthy and happy.
Throughout September we’re offering you the chance to take the first step to a healthier future with a free women’s wellness assessment. During your free women’s wellness assessment, you will be able to speak to one of our resident osteopaths who have years of experience behind them find out where you need some extra support and lend a helping hand.
If this sounds like the answer to the pain that you’ve been searching for, arrange your free women’s wellness assessment by filling in our simple web form or call our Mount Waverley or Murrumbeena clinic at 1300 003 007 and a member of the team will be happy to help!
Other Free Resources For Women’s Health
Are you in the early stages of pregnancy right now? Why not download our free pregnancy-related pain report to get 7 ways to journey through pregnancy including support to empower yourself and your little one to prepare for labour and recover well after birth?
Download Your Copy Of Our FREE Pregnancy-Related Pain Report Here!
Read Our Blog – What Pelvic Floor Exercises Should I Actually Be Doing?